BY EILEEN STUKANE | Life as they know it changes for women when they learn that one of their two Breast Cancer (BRCA) genes — which is supposed to offer cancer protection — has a mutation, a glitch that causes an increase in their risks of developing breast and ovarian cancer.
During this October Breast Cancer Awareness Month, a number of women who have tested positive for BRCA1 or 2 mutations have shared the pathways they have followed to reduce their risks and live their best lives. Many have turned to the organizations SHARE Cancer Support (visit sharecancersupport.org or call 844-ASK-SHARE), a unique self-help organization for women with breast or ovarian cancers, and Facing Our Risk of Cancer Empowered or FORCE (visit facingourrisk.org or call 866-288-RISK), a grassroots organization dedicated to improving the lives of women who have hereditary breast, ovarian, and related cancers.
The American Cancer Society (cancer.org) estimates that in 2017 there will be an estimated 252,710 new cases of invasive breast cancer and 63,410 in situ cases, totaling over 315,000 women being newly diagnosed with breast cancer in a year where an estimated 40,610 women will die from the disease. (There will also be 2,470 cases of breast cancer diagnosed in men.) Breast cancer remains the second leading cause of cancer death in women, the first being lung cancer.
Statistically in the USA, a woman has about a 1 in 8, or roughly 12 percent risk of developing breast cancer in her lifetime. Women who have a BRCA1 or 2 mutation (or both) can have up to an 80 percent risk of being diagnosed with breast cancer during their lifetimes, usually when they are in their younger premenopausal years, and the cancer can appear in both breasts more often for them than for women who do not have the abnormal genes. (In addition, American Cancer Society statistics show that the risk for developing ovarian cancer by age 70, jumps from less than 2 percent in the general population, to 35–70 percent for the BRCA1 mutation, and 10-30 percent for the BRCA2.)
Although less than 1 percent of the US general population carry the BRCA gene mutations, they are about 10 times more common among women of Ashkenazi Jewish descent, and also high among Norwegian, Dutch, and Icelandic populations. Women seek out genetic testing (through blood or saliva) when they recognize a family history of breast and ovarian cancers (which was the case for actor/director Angelina Jolie), or they are diagnosed with a breast or ovarian cancer themselves. The abnormal genes can be passed from generation to generation either by a mother or a father, and each daughter or son has a 50/50 chance of acquiring them. Testing positive for one of the mutated genes then calls for inner strength and courage as cancer risks increase before a woman’s eyes and decisions involving whether or not to undergo extensive surgery must be made.
CHALLENGES AND CHOICES | A breast surgeon who sits across from a woman who has tested positive for the BRCA1 or 2 gene mutations will undoubtedly tell her that she can undergo a preventive double mastectomy, technically a “bilateral prophylactic mastectomy,” with reconstruction if she chooses, and she will reduce her risk of developing breast cancer by 90 percent. If she chooses not to have this surgery, she has the option of careful monitoring, alternating every six months between mammography screenings and MRIs, to detect any changes in her breast tissue. In some cases, drugs such as Tamoxifen or Raloxifene are recommended.
Christine Benjamin LMSW, Breast Cancer Program Director at SHARE, was diagnosed with early stage breast cancer at age 36 in 2000. At the time, she did not know she carried the BRCA1 gene mutation. The BRCA1 gene mutation was discovered in 1994, and the BRCA2 in 1995. In 2000 they were still being researched, and health insurance companies had not yet gotten around to covering genetic testing. Benjamin entered a study at Memorial Sloan-Kettering and learned she had the abnormal BRCA1 — which meant she had to go beyond standard treatment for breast cancer.

Grappling with issues of body image, some women who learn of their gene mutations would rather do the precision monitoring than have a preventive double mastectomy. Benjamin felt differently. “It was more about lifestyle and what I thought I could handle emotionally,” she recalled. “From the time I was diagnosed to the time I had surgery I think I had 18 doctor appointments, just a gazillion appointments, and I just thought, I don’t want to live my life this way.” She had the preventive double mastectomy, chemotherapy, and reconstruction. A year later she underwent further surgery. “I felt I needed to be as proactive as I could,” Benjamin said, “not that there was any evidence, but I had my ovaries and fallopian tubes removed.” Without hormone-producing ovaries, a woman reduces her risk of breast cancer. Benjamin, who had no children but was in a relationship, had deep discussions with her partner over this life-changing decision: “I remember feeling like I really needed to do this, it was very clear to me.”
Benjamin, like the rest of the women in this article, emphasized that there is no “right” decision about how to proceed since science cannot yet predict what the future holds. “If you knew that when you’re 78 you’re going to develop some kind of cancer, would you do anything prophylactically now? Science is just not there yet,” she said. However, today, SHARE and FORCE have many peers who have gone through the process and are there to help. “People don’t have to go through it alone,” she noted, recalling, “I had to do it alone.”
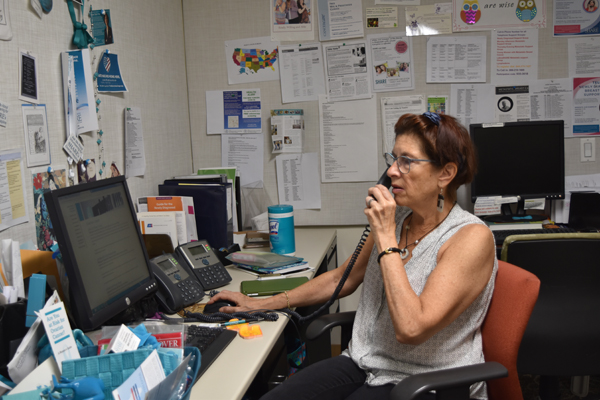
Andrea Herzberg, Ovarian Cancer Helpline Coordinator at SHARE, also recommends that women with BRCA1 or 2 mutations reach out to women at SHARE and FORCE. Herzberg herself learned at age 43 in 2000, at the time when she had a nine-year-old daughter, that she carried the BRCA2 gene mutation. She had been diagnosed and treated for late-stage ovarian cancer prior to finding out. She decided that since her total hysterectomy and chemotherapy had already lowered her risk of breast cancer, unlike Benjamin, she would opt for surveillance through the screenings.
“Women who discover that they have increased risk of breast or ovarian cancer, are going to come at the decision-making process from different perspectives, based on their own individual, personal situations. At SHARE we encourage everyone to make informed decisions,” Herzberg said. “By the time I was 40 I had had two major surgeries, a lot of chemotherapy. Unlike ovarian cancer, breast cancer has early screening.” She decided to follow through on surveillance screenings, and has done so for the last 17 years. “I decided I could live with the increased surveillance. I didn’t want to run after more surgery unless I needed it and this turned out to be a plan for me.”
It is not uncommon for women at high risk to say they have reached a certain level of tolerance with surgical intervention, and therefore prefer breast surveillance through screenings. Deborah Polinsky LCSW, mental health therapist and volunteer at SHARE and FORCE, had a response similar to Herzberg’s. Polinsky did not know that she carried the BRCA1 mutation when she was diagnosed with late stage ovarian cancer in 2006 at age 52, but learned shortly thereafter. When the surgery and chemotherapy treatments for her ovarian cancer left her with chronic neuropathy, nerve damage that causes pain, in her hands and feet, she did not want to go through any further surgery. She chose to have surveillance through breast screenings rather than undergo a preventive mastectomy, a decision reached after consulting with genetic counselors who researched statistics for her.
“Their data showed that as you get older the risk of breast cancer due to genetic mutation comes closer to the risk for women in the general population. If you find out when you’re 25 that you have this (a gene mutation) then you have all those years of being at risk, but I was already in my 50s,” Polinsky said. Based on the medical literature, which also showed that the screenings could identify early stage breast cancer and overall survival rates were similar to those of older women in the general population, Polinsky concluded that she was comfortable with surveillance through screenings. Eleven years later, she has not shown any sign of breast cancer.
Every high-risk woman is really on her own in charting her future. Linda (who did not want her last name used) was diagnosed with ovarian cancer at age 47 and she felt similarly to Deborah Polinsky. After surgery and chemotherapy, and learning she carried the BRCA2 mutation, her inclination was to refrain from further surgery. She decided to do breast surveillance through screenings, but also took the drug Tamoxifen as a preventive measure. When she reacted badly to the drug, she changed her mind and chose to undergo a preventive bilateral mastectomy with reconstruction using silicone implants. Her breast surgery revealed atypical lobular hyperplasia, distorted cells within her breast that are a sign of an increased risk of breast cancer, and these cells cannot be detected though imaging. Linda’s change of course turned out to be the right decision for her.
Life experiences, relationships, support groups, and medical experts create a mix that for each woman is different. Herzberg made the important point that women who have witnessed family members die before age 40 due to hereditary genes, approach their decision-making differently than women who have not had these experiences: “Having the mutation doesn’t mean you’re definitely going to get cancer,” she noted, “but having spoken to women through the SHARE Helpline, I think some cannot live with that sword of Damocles and they’ll make a decision.”
Jane Herman, writer/editor for the Union for Reform Judaism and a Peer Support Group Leader for FORCE, sought genetic testing at age 47 in 2010 after her mother died of metastatic breast cancer. Even though her mother passed away in her 70s, Herman knew of the higher risk among Ashkenazi Jews. She was fortunate to have followed her instincts. She tested positive for a BRCA2 gene mutation and underwent a full hysterectomy in 201o to lower her risks. After that surgery her intention was to follow through with breast surveillance. She had never been diagnosed with a cancer but when she was diagnosed with the abnormal gene she “used to tell people that I fall asleep every night thinking about breast cancer and I wake up every morning thinking about breast cancer. I was convinced I had it and it was growing.”
When her first MRI first showed something suspicious, Herman underwent more testing, an ultrasound, and a needle biopsy. “I spent more time having tests than I could ever have imagined,” Herman recalled, “and that was a real eye-opener for me to realize that I didn’t have the personal tolerance to do this every six months for the rest of my life.” She made the decision to undergo a complete prophylactic bilateral mastectomy with breast reconstruction using her own transferred abdominal tissue. It was a 12-hour surgery. Today she says that the decisions she made “were absolutely the right decisions for me. I came to this having watched my mother decline within seven weeks, from being active and not ill, to being in a hospice.”

Every woman’s story is unique. Annie Brickel, a retired New York City educator and a Peer Support Group Leader for FORCE, lost her 42-year-old mother to ovarian cancer when she was eight years old in the 1950s, when the mutated genes were still unknown. In more recent years, her NYC doctor persisted in telling her to be genetically tested. In 2010, she relented and learned that she was positive for the BRCA1 mutation. She found emotional support through FORCE volunteers who also gave her research information and direction.
Brickel, who is the mother of fraternal twin daughters and a son, had undergone a complete hysterectomy in 1994 due to the foresight of her physician who knew her family history, so her breast cancer risk had already been reduced. However, one twin daughter and her son also tested positive for the mutated gene. Brickel and her daughter Carrie chose to follow through with the mammography/MRI screenings on alternating six months until 2013 when, at age 36, Carrie was diagnosed with a stage 1 triple negative breast cancer, and her doctor said she had six weeks to make surgical decisions. “Even though I wasn’t the one with the cancer, you’re watching your child go through this and it takes an emotional toll. It’s a very helpless feeling. But I did know that when she was finished with her journey that I was going to become very proactive with mine,” Brickel said.
Carrie underwent extensive surgery that included a bilateral mastectomy with reconstruction using a tissue-transfer from her own abdomen, a procedure called DIEP (deep inferior epigastric perforator) flap surgery. She is in good health today. Brickel then changed her approach to dealing with her own situation and in 2014 chose to do a preventive bilateral, nipple-sparing mastectomy with reconstruction using adjustable saline implants. The implants are slowly expanded through tubes that are removed when the expansion is complete. Brickel hopes that by the time her son’s children are adults there will be medical breakthroughs in ways to manage the genetic mutations.
MORE FINDINGS FROM GENETIC TESTING | Since the BRCA1 and BRCA2 genetic discoveries, over a dozen more genetic mutations have been found to affect the risk of breast cancer, and more are being researched. These genetic discoveries will help to individualize the way cancer is treated. For women already diagnosed with genetic mutations, however, an “individual” approach has always been the way.
Eileen Stukane is a frequent contributor to Chelsea Now. She is co-author of “The Complete Book of Breast Care” (available at amazon.com). Her ebook memoir, “Running on Two Different Tracks,” published by Shebooks, is available at amzn.to/1PqZens.